Before Zachary Wolkoff was a year old, he’d already made many trips to the Manhattan emergency room, covered in welts and hives. No one could figure out the cause. At the time, his mother, Stephanie Winston Wolkoff, now 44, was exclusively nursing Zach, so a reaction to food seemed unlikely. But an allergist cleared up the mystery. “We were eating nuts,” says Wolkoff, and when we would touch his skin, the oils from the nuts would cause him to break out.”
As Zach got older, the tiniest trace of nuts—even from a knife that was used to cut a peanut butter sandwich and then his food—could cause anaphylaxis. Zach’s throat would close up and he’d have trouble breathing. A few months after his second birthday, Wolkoff ordered takeout, asking that no nut oil be used. When dinner arrived, Zach grabbed a french fry off his mother’s plate and took a bite. A few minutes later, when Wolkoff was putting Zach in his crib, he fussed about his eye. Luckily, she checked on him later. “When I went in there, there was no face,” says Wolkoff. “He was deformed and swollen. I wrapped him in a blanket and ran downstairs.” She took Zach to the E.R., where doctors gave him shots of epinephrine and steroids, which saved his life.
Zach survived, but has spent much of his 12 years living in fear—rarely eating out and limiting activities with friends—as he navigates the often-lonely existence of living with food allergies.
And he’s not alone. The number of children being diagnosed with food allergies has exploded over the past 20 years, worrying doctors, moms and schools alike. Milk, eggs, peanuts, tree nuts, soy, wheat, fish and shellfish account for 90% of all reactions. Not all food allergies are life threatening, but peanuts, tree nuts, seafood and even milk are responsible for a disproportionately high rate of anaphylaxis, a dangerous reaction in which the flood of chemicals released by the immune system leads to a rapid narrowing of the airways. Researchers estimate that in the U.S., up to 17 million Americans have food allergies and they have an impact on 1 in every 12 children under the age of 21. In Australia, 10% of 1-year-olds are affected.
The spread of allergic reactions reported in kids has been shocking: a 50% increase between 1997 and 2011, according to a CDC study released in 2013. The rate of people with food allergies is doubling approximately every 10 years warns the CDC, and the incidence of peanut allergy alone has tripled between 1997 and 2008. The rise in eczema and asthma has gone hand-in-hand with this allergy outburst. And no one really knows what’s causing it.
Fortunately, doctors are on the cusp of some dramatic breakthrough treatments, with oral immunotherapy (OIT) leading the way. During OIT—a method used essentially to train the immune system not to overreact—a patient ingests the food allergen in small but steadily increasing doses, until he or she is desensitized to it. While recent clinical trials have shown that OIT is effective in about 80% of patients if administered by a doctor and the person continues eating the allergen regularly, it’s still not clear whether full tolerance is possible. But in a breakthrough study, scientists have shown that giving infants bits of peanut protein over time could circumvent a peanut allergy altogether.
While OIT isn’t FDA-approved and therefore not offered as a widespread treatment yet—and there’s much controversy surrounding whether it should be—Zach is one of the lucky few participating in a clinical trial at Stanford University combining OIT with a powerful drug called Xolair, an asthma medication being investigated for allergy use. The goal is to desensitize him to peanuts, cashews, pistachios and hazelnuts all at the same time—with the hopes of him eventually losing these allergies altogether.
The Emotional Toll of Living with Food Allergies
 ntil recently, kids like Zach had only one way to deal with a food allergy: strict avoidance (which sounds simple, but isn’t) and keeping at hand an EpiPen, a shot filled with epinephrine that is the only known way to halt a potentially deadly reaction. For Zach that meant shunning any packaged food that said somewhere in tiny writing: “made in a factory with nuts.” He also had to be wary of all forms of cross-contamination, through cooking utensils, cooking surfaces or a frozen yogurt machine that had a peanut butter flavor in it earlier. It’s a tall order for a 12-year-old.
ntil recently, kids like Zach had only one way to deal with a food allergy: strict avoidance (which sounds simple, but isn’t) and keeping at hand an EpiPen, a shot filled with epinephrine that is the only known way to halt a potentially deadly reaction. For Zach that meant shunning any packaged food that said somewhere in tiny writing: “made in a factory with nuts.” He also had to be wary of all forms of cross-contamination, through cooking utensils, cooking surfaces or a frozen yogurt machine that had a peanut butter flavor in it earlier. It’s a tall order for a 12-year-old.
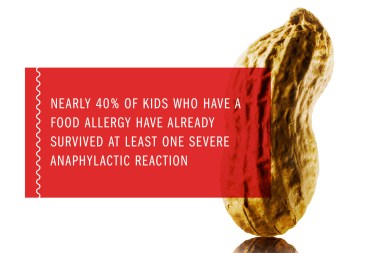
A 2010 survey of 40,000 U.S. parents found that nearly 8% percent of children under the age of 18 have a food allergy. The researchers also found that nearly 40% of kids who have a food allergy actually have already survived at least one severe anaphylactic reaction. For families navigating food allergies, the fear of death is constant and just a bite away.
Understandably, Zach suffered from extreme anxiety around food. “I would be scared that I would have to use the EpiPen or go to the hospital and I may die,” he says. He never joined friends for ice cream, and skipped most baseball games (peanuts everywhere), movie theatres (popcorn is sometimes made in peanut oil) and plane rides (peanuts are the go-to snack.) “Vacations were a nightmare,” says Wolkoff. “I couldn’t get on a plane without him having a panic attack for fear other people would be eating nuts.” She’d ask the flight attendant to make an announcement and board early to wipe everything down. “I had to clean the seats, the trays, the lights, even the doors on the bathroom.”
Every four minutes, a food allergy reaction sends a child to the emergency room. Reactions happen quickly and it’s not always obvious when to administer the EpiPen. Natalie Giorgi had a mild reaction to peanuts at age 3 and never showed symptoms again until the night she died two years ago, age 13, after eating a Rice Krispies Treat that had peanut butter in it at a party. She sat with her parents and appeared fine right afterwards, but within 20 minutes she was vomiting and struggling to breathe. By the time her father administered two EpiPens it was too late.
According to Dr. Kari Nadeau, associate professor at Lucile Packard Children’s Hospital, Stanford and Stanford University School of Medicine, who is treating Zach, only 55% to 60% of people with food allergies always carry an EpiPen. Benadryl helps with rashes, but can’t prevent anaphylaxis. If a person is wheezing, turning blue or throwing up with hives, use the EpiPen—it can’t hurt. She advises families to have two Epis at all times, because the reactions are so unpredictable. “You can have one type of reaction one day, but then there is a 25% chance of having a completely different reaction to the same amount of food on a different day,” says Nadeau. “If you have a virus or if you’ve taken a hot shower or if you’ve just exercised or been out in the hot sun, that changes your threshold and you could have a full-blown reaction.” In other words, daily life matters. Even a low immunoglobulin E (IgE) test, a blood test to check whether someone is allergic to a substance, doesn’t necessarily mean that person will have a mild response.
For all the week’s parenting news, sign up for Time for Parents, a free weekly newsletter, here.
What’s Causing the Allergy Epidemic?
 o one knows for sure what’s behind the dramatic escalation in food allergies. What scientists do know is that a child’s risk has a genetic component: the chances of having a food allergy are 65% greater if a kid has a parent or sibling with any type of allergy (even an environmental one like hay fever). The propensity for allergies, not necessarily the type, is what’s passed down. Peanut and tree nut allergies are usually life-long, while kids can outgrow reactions to milk, soy and eggs. Still, those foods can cause deadly reactions too and studies show that kids are taking longer to outgrow them.
o one knows for sure what’s behind the dramatic escalation in food allergies. What scientists do know is that a child’s risk has a genetic component: the chances of having a food allergy are 65% greater if a kid has a parent or sibling with any type of allergy (even an environmental one like hay fever). The propensity for allergies, not necessarily the type, is what’s passed down. Peanut and tree nut allergies are usually life-long, while kids can outgrow reactions to milk, soy and eggs. Still, those foods can cause deadly reactions too and studies show that kids are taking longer to outgrow them.
Scientists believe our surroundings and epigenetics —how the environment alters genetic inheritance—must be at work. In the U.S. alone, the prevalence of peanut allergies went from one in 250 kids to one in 70 kids from 1997 to 2008, according to a survey done by Dr. Hugh Sampson and Dr. Scott Sicherer of the Jaffe Food Allergy Institute at Mount Sinai Hospital in New York City. “It’s so short of a time frame,” says Sicherer. “It has to be that something about the environment has changed.”
So, what’s different? Well, everything. Kids don’t play outside as much as they used to and are less exposed to sun and vitamin D, which may be linked to proper immune function. Also, “Family sizes were larger, kids used to be playing in the dirt, and weren’t washing their hands frequently,” says Sicherer. Since we’re living in cleaner environments—all that antibacterial soap—and use antibiotics liberally, our immune systems aren’t working as hard to fend off all the germs and diseases. “Maybe our immune system needs something to chew on so it’s now attacking the wrong thing,” says Sicherer. Still, the hygiene hypothesis, as this theory is known, can’t explain everything, since allergies are on the rise in many Western nations— even in some of the most unsanitary environments. “The highest incidence of asthma, which is often related to allergies, is in Spanish Harlem in New York City, a place full of dust mites and toxins,” says Dr. Aimee Altschul-Latzman, an allergist-immunologist in Fairfield, CT. “The hygiene theory doesn’t completely hold up.”
As a tie into the hygiene hypothesis, doctors point to the rise in C-sections as a potential risk factor, since the delivery is more sterile than a vaginal birth. Babies delivered by C-section don’t receive the protective vaginal flora from the mother’s birth canal, which has some moms asking that their babies be swabbed with bacteria from the vagina. “What happens at birth sets your baby’s immune system for life,” says Dr. Wesley Burks, chair of the Department of Pediatrics and physician-in-chief of North Carolina Children’s Hospital and a proponent of this view.

One study showed that handwashing dishes (less sterile than using dishwashers), was linked to a lower allergy risk. And too much folate may increase your—or your baby’s—risk too. The rise in allergies corresponds with expectant mothers being first advised to ingest 800 mg of folic acid 20 years ago. And just as antibiotics can knock off the good bugs in our gastro-intestinal tract, soap affects our skin. “Don’t bathe babies all the time,” advises Dr. Sampson. “Try not to wash off all the bacteria because some is protective.”
Dr. Robert Wood, a chief of Pediatric Allergy and Immunology at Johns Hopkins Children Center, cautions against placing too much emphasis on any one theory, since it’s most likely a combination of things. “C-sections show up as being statistically significant only if you look at a lot of babies,” says Wood. “I wouldn’t tell women to stop folate and not have C-sections.”
So what can parents do? Pay attention to diet during pregnancy and the child’s diet during the first few years. “It seems like the microbiome [or bacteria] in the gut get into the placenta a little bit,” says Nadeau, “and they are educating the child’s immune system while you’re pregnant.” Expectant moms should eat a healthy, Mediterranean-style diet, including fish, fruits, vegetables, olive oil and yogurt while making sure to get plenty of Vitamin D and calcium; cut back on fast food, sugars and saturated fats. Dr. Altschul-Latzman tells expectant mothers to eat peanuts and nuts as usual, especially during the third trimester when the baby’s immune system is forming, but don’t overdo them. And breastfeeding for six months is thought to be protective.
As for feeding your baby, “diversifying the diet for your kid is going to be key,” says Dr. Nadeau. There’s evidence that introducing rice cereal and corn before six months increases the allergy risk, while offering wheat, eggs and fish before nine months decreases it. And in February, a surprising study found that many peanut allergies can be avoided by feeding your infant peanut-laden foods (like peanut butter) between four and 11 months, rather than avoiding them. This completely goes against guidelines from 2000 telling parents to withhold peanuts from children until age 3, which may have contributed to our allergy epidemic. What’s most significant about that study is that all groups who ingested peanuts, even those infants who had already had a reaction, had a lower peanut allergy rate at age 5 than the group that skipped peanuts altogether. (Be careful, though. High-risk infants should have a skin-prick test between four and eight months before ingesting peanut protein.) What’s more, another February study showed that giving peanut OIT to toddlers under age 3— whose immune systems are still developing—was most effective, as 97% of them beat their allergies.
The Frontiers of Treatment
 n 2012, Wolkoff heard Nadeau speak at a Food Allergy Research and Education (FARE) lunch about her experimental treatment using OIT, where patients eat increasing doses of an allergen to train their bodies not to react. She was intrigued. But, when she ran it by Zach, his response was: “No way.”
n 2012, Wolkoff heard Nadeau speak at a Food Allergy Research and Education (FARE) lunch about her experimental treatment using OIT, where patients eat increasing doses of an allergen to train their bodies not to react. She was intrigued. But, when she ran it by Zach, his response was: “No way.”
Wolkoff spent the next year researching the treatment, and when Nadeau was in New York City again, she had her over to her apartment along with Kim Yates Grosso whose daughter Tessa was the first person to be treated with OIT for multiple foods at once—Nadeau’s specialty. Zach liked Nadeau’s reassuring nature and he bonded with Tessa over their food fears. “I was terrified to do the treatment,” he says, “but I thought if it can change Tessa’s life it can change mine too.”
The food allergy community around Nadeau is tight-knit. Many patients have become friends with each other, staying at each other’s houses and texting each other moral support. And Nadeau, a mother of five, fits right in. She takes calls at any time of night, even while on vacation, and throws parties once her patients have completed a study. The success of her multi-allergen treatment has gained her worldwide attention. In January, Sean Parker of Napster fame, who suffers from severe food allergies, pledged $24 million over the next two years to Stanford University School of Medicine to set up a center led by Nadeau to continue and share her research. Jeff Bezos of Amazon pitched in another $2.25 million.
On Jan. 6, 2014, Zach flew out to Palo Alto for two weeks to test his allergies, ingesting just enough of each of his allergens to stir a reaction. At only 5mg, (equal to a speck) his lips started to swell and his stomach hurt. After two weeks, Zach took his first of five shots of Xolair, which blocks the IgE antibody that causes anaphylaxis, so he could increase his treatment doses more rapidly. Patients on Xolair can complete the protocol in as little as six months, instead of three years. Every two weeks Zach would fly out to California and get a 25% updose, or increase of his allergens, while doctors monitored his reactions. If he didn’t have any symptoms, he would take home that amount (in capsules because he hated the taste) to eat every night.
While some kids sail through the treatment, nothing about this was easy for Zach. He often needed hours of persuading to take his dose, which at first made his stomach hurt, and he refused to leave the house afterward for fear he’d have a reaction. Sometimes he’d throw up, but wasn’t sure if it was just nerves. Of the 700 patients whom Nadeau has treated this way, Zach had the toughest time emotionally. But three months into his treatment, he no longer had to worry about cross-contamination from nuts. By the end of August 2014, he was desensitized completely: his IgE level , the amount of antibodies in the blood that attacks allergens, showed that he was no longer allergic.
Zach used to ingest all four nuts daily, but six months after he finished treatment, he only had to eat one type every three days to stay desensitized. Nadeau tries to ensure that a patient can get up to 2 grams of peanut protein (a tablespoon of peanut butter) a day without symptoms. And while she emphasizes that this is not a cure—many of her patients must continue eating their allergens daily to keep up their tolerance—she’s had others who have beat their allergies completely, at least for now. What happens five years out is still an open question. “It’s going to take people coming back and getting retested,” says Nadeau. “There does seem to be a switch for each person that if they cross that threshold they could have a more permanent response.” She tells every patient still to carry an EpiPen.
OIT isn’t without controversy. It’s still in phase 2 clinical trials and at least six years away from FDA-approval. Obviously, no one should try it without a doctor’s supervision. “There’s no way I’d do it,” says Johns Hopkins’ Wood, who has a severe peanut allergy. “I am fully aware that I will have more reactions in my life, but if I went through OIT I would have a lot more reactions going through the treatment. And I don’t think it has gone through sufficient study yet.” He worries that patients might not maintain regular exposure to the food, since many hate the taste, and then might not be prepared for a reaction.
Still, a few places, like the New England Food Allergy Treatment Center in West Hartford, Connecticut, offer OIT as a treatment—not just a clinical trial—and most Connecticut insurances will cover it. The Center has treated over 550 patients the past 4 years with more than 90% becoming desensitized, according to the Center. “It can have a tremendous impact on the quality of life,” says Dr. Jeffrey Factor, medical director of the Center. “Only about 5% of patients required an EpiPen during the buildup process, which is a very low number.”
Other treatments in the pipeline might prove as beneficial, but they haven’t been studied as long. Dissolving a small amount of the allergen under tongue the allows patients to ingest up to about two peanuts and appears to have fewer side effects, but isn’t as protective. Exposing patients to a small dose of peanut protein through a patch can get them to increase their tolerance to up to about five peanuts with seemingly minimal side effects, but more research is needed into whether the effect lasts. At the moment, OIT lets patients tolerate more of the allergen and probably has the longest-term benefits. But it tends to have more side effects.
For Zach, who could never have completed the treatment as safely without the help of Xolair, the dream of living a normal life has already come true. In addition to eating one new food a day, he has gone bowling, to the movies and on multiple plane rides. “Before I would have been sitting in the house when everyone else was eating out because I was too scared,” he says. “Now I feel more comfortable going out with my friends.” And no one is happier than his mom. “We can take a deep breath for the first time in our lives.”
Five Helpful Links
What To Do When Your Toddler Has a Sudden Allergic Reaction